Base of Thumb Arthritis
In a normal joint, cartilage covers the ends of the bones, and allows them to move smoothly and painlessly against one another. There is also fluid within the joint which helps to provide lubrication and nutrients to the joint. In osteoarthritis, inflammation and damage to the joint cartilage over time can cause pain, and a reduction in joint space. The ligaments
which support the joint can become often lax and less supportive, allowing the joint to slightly slip out of place (become subluxed), resulting in abnormal positioning of the joint.
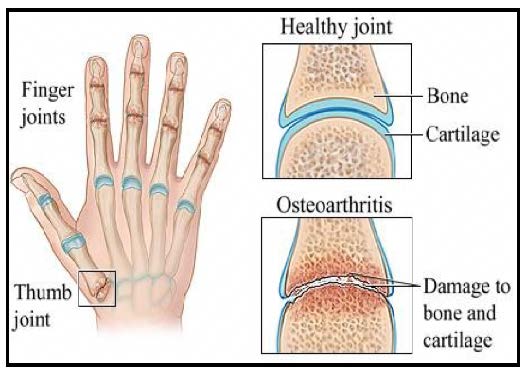
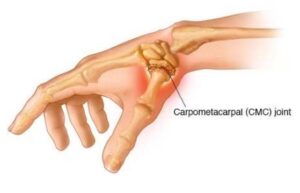
It is quite common to develop osteoarthritis in the base of the thumb, specifically in the carpometacarpal (CMC) joint. The specialised saddle shape of this joint allows the thumb a wide range of movement.
Risk Factors
- Past injuries to the joint such as fractures or sprains
- General joint laxity or hypermobility
- Repetitive activities
- Genetic / family history
- Women can develop arthritis more commonly than men
Symptoms
- Deep, aching pain or feeling of stiffness at the base of the thumb – this can occur with use, at rest and at night time
- Loss of strength resulting in difficulty with activities that involve gripping or pinching – e.g. turning a key and opening a door
- An aching discomfort after prolonged use
- Swelling and tenderness at the base of the thumb
- Limited motion
- An enlarged ‘out-of-joint’ appearance
- Development of a bony bump at the base of the joint
Diagnosis
Arthritis can usually be determined by a visual / physical assessment, however X-ray can be used to confirm the extent of physical changes within the joint. If your doctor suspects that you may have rheumatoid arthritis (which is different to osteoarthritis), you may be asked to have some blood tests.
Conservative Management
Conservative management is usually indicated in mild to moderate cases. Arthritis is not curable, however treatment aims to reduce pain, support and protect the joints and strengthen supporting muscles. It also aims to maintain and improve range of movement, promote functional activities and help to develop self-management strategies.
You may find relief from the following:
- A soft, semi – rigid or rigid splint. These can be splints to wear during tasks or a rest, which can either be custom made by your therapist or purchased off the shelf
- Applying moist heat (e.g. heat wheat or paraffin wax bath) when joints are painful
- Dynamic stability exercises and gentle strengthening (your therapist will prescribe these if appropriate)
- Radial nerve glide exercise
- Heat controlling gloves e.g. IMAK Arthritis gloves – especially in the colder months
- Compression or oedema control e.g. Isotoner gloves
- Joint protection principles and work simplification strategies
- Assistive devices e.g key turners, jar openers
- Anti-inflammatory medication – speak to your GP
- Corticosteroid injections
Surgical Management
When conservative management is no longer effective or indicated, surgery is another option. A variety of surgical techniques are available that can successfully reduce or eliminate pain, improve thumb position and maximise function. Hand therapy is typically prescribed post-surgery to ensure the best functional outcomes.