What is Camptodactyly?
Camptodactyly is a non-traumatic flexion contracture of the proximal interphalangeal joint (PIPJ), most commonly affecting the little finger, although additional fingers may be involved.
The contracture generally increases during growth spurts especially during the periods of rapid growth (age one to four years, and age 10 to 14 years)1
The contracture is painless, and patients typically present with concern over appearance or functional limitations.
The patient and family should be advised that treatment is long and follow-up throughout the skeletal growth period is necessary; and after partial or total correction, relapses may occur.1

Cause
The exact cause remains debatable. Theories include fourth lumbrical anomalies or absence, palmar interossei anomalies, hypoplastic FDS, lateral band adherence, inability of the volar skin to stretch during rapid growth, and a congenital absence of the central slip. Assessment of all potentially involved structures should be considered.2
Classification
Benson et al in 1994 classified Camptodactyly as1:
Type I: Infantile. The most common form, becomes evident during childhood. It generally affects the little finger alone, and affects boys and girls equally.
Type II: Adolescent. Camptodactyly of adolescence (between ages seven and eleven years), which occurs predominantly in females. It tends to start subtly and evolves gradually and progressively. It affects girls more than boys. Does not improve spontaneously and may evolve to severe flexed deformity.
Type III: Syndromic. Present from time of birth. Usually affects several fingers, is bilateral and associated with a variety of syndromes.
Differential Diagnosis
Traumatic injuries, family history and other congenital anomalies should be assessed. Differential diagnoses include: traumatic Boutonnière deformity, Dupuytren’s contracture, trigger finger, extensor mechanism absence, neurogenic clawing, and arthrogryposis.2 An Xray may be indicated to rule out other pathology and to detect articular change.3
Conservative Treatment
Managing patient/family expectations is important. Adherence to a passive stretching and splinting protocol can achieve an acceptable result. It is important to educate families that the contracture worsens during periods of rapid growth.2
Yannascoli & Goldfarb have recommended four components for conservative management.
- Passive stretching (isolated PIPJ extension, at least four times a day for 5 minutes).
- Active extensor strengthening (PIPJ extension with MCPJ flexion: isometric, using rubber bands or extending into putty).
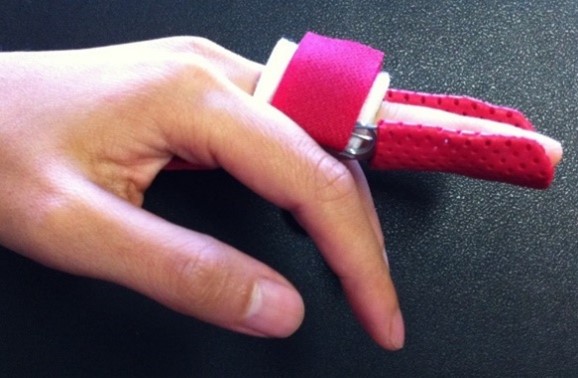
- Night time static progressive orthosis (for nap time or bedtime, under 8 years old needs wrist included to prevent migration, hand-based for over 8-year-olds, tape may be required). PIPJ in maximum extension. MCPJ and DIPJ hyperextension to be avoided. This may be the only orthosis required for a contracture of 30 degrees or less.

- Dynamic finger orthosis (i.e. capener orthosis) recommended for adolescents with contractures of 45 degrees or less, who are very active during day and unlikely to comply with stretching and active extensor strengthening protocols benefit most from this orthosis
Surgery
Surgery is indicated for fixed contractures that interfere with function, that have not resolved with a three-to-six-month trial of supervised orthosis wear, and for contractures of 60 degrees or more.4 Lack of compliance with conservative therapy should alert the surgeon that postoperative compliance may also be compromised. Surgical options range from release of tendons or facial bands, tendon transfer, and tenotomy.5
Trivia
The term Camptodactyly stems from a Greek work translated as ‘bent finger’.2
- The most commonly involved digit is the small finger, followed by the ring finger, index, and then middle.
- Camptodactyly affects approximately 1% of the population
- It is bilateral in about 2/3 of patients, although the degree of contracture is not always symmetrical.1
- There is an equal sex distribution in the infantile presentation, whereas girls are more commonly affected when the condition presents in adolescence.
Case Study:
In a recent case study at Gold Coast Hand Therapy, “Anna” a 12-year-old female presented with right small finger Camptodactyly. She was referred via a paediatric orthopaedic surgeon, who had completed a comprehensive assessment including Xray and ultrasound, before referring to hand therapy for splinting. Anna was born with a ‘bendy’ little finger (ie Type I). Her PIPJ had an extension lag of 60 degrees, with shortening of the volar skin; however her joint was not contracted and was passively correctible to 0 degrees with her MCPJ flexed. As she had a lag rather than a contracture, a cylinder orthosis was made for day wear as much as possible, and a hand-based orthosis for night time (with MCPJ flexed and IPJs in full extension). She was reviewed after three weeks and her lag had improved to 25 degrees. Her orthoses were adjusted to accommodate these changes. She was advised to remove her cylinder orthosis during the day for functional activities and handwriting, and continue with her night time orthosis. Three weeks later her finger had improved to having a 20 degree lag. A relative motion orthosis was worn during the day to strengthen the central slip (she had a 10 degree lag with RMS insitu), and she was advised to continue with her night orthosis. She was a very compliant patient with an excellent outcome. Due to predicted growth patterns, she may need to continue with the orthoses during her adolescence, and return to hand therapy if there are any problems.
Outcome after six weeks of splinting, at the third hand therapy appointment:


References:
- Almeida, S.F., Monteiro, A.V., da Silva lanes, R.C., (2014). Evaluation of treatment for camptodactyly: retrospective analysis on 40 fingers, Revista Brasileira de Ortopedia, 49(2), 134-139.
- Yannascoli, S.M., Goldfarb, C.A. (2018). Treating congenital proximal interphalangeal joint contracture, Hand Clinics, 34, 237-249
- Comer, G.C. & Ladd, A.L. (2015). Management of complications of congenital hand disorders, (2015). Hand Clinics, 31, 361-375.
- Wall, L.B, Ezekiel, M., Goldfarb, C.A. (2018). Camptodactyly treatment for the lesser digits, Journal of Hand Surgery Am, 43(9), 874.e1-e4.
- Singh, V., Haq, A., Puja, P. & Kumamoto, P. (2018). Camptodactyly: an unsolved area of plastic surgery, Archives of Plastic Surgery, 45(4), 363-366