There is consensus in clinical practice and the medical literature that splinting for De Quervains Tenosynovitis can improve symptomalogy. It is accepted practice that the wrist and thumb (excluding IPJ) need to be influenced by the splint in order have effect on the Extensor Pollicus Brevis (EPb) and Abductor Pollicus Longus (APL) tendons. However, there is very little consensus on splint design with many iterations being offered to patients.
De Quervains tenosynovitis is now understood to be more of a tendinosis rather than a tendinitis/tenosynovitis, with histopathology studies finding myxoid degeneration rather than acute inflammatory cells (Pensak et al, 2013). The tendons involved are the Extensor Pollicus Brevis and Abductor Pollicus Longus as the 1st dorsal compartment and then under the extensor retinaculum at the wrist. The mechanism of degeneration remains unclear and it is proposed that repetitive movements of the wrist and thumb, specifically ulna deviation in combination with thumb flexion-extension-abduction and/or opposition eg turning a door handle, turning a tap, produces micro-tears which may cause collagen disorientation, mucoid changes and thickening of the extensor retinaculum (Pensak et.al 2013). Splints are generally aimed at reducing the repetitive movements of the thumb and wrist and local steroid injections are frequently used in combination with splinting.
It is now generally recognised as a self-limiting process in the majority of patients and those with concurrent depressive symptoms are strongly correlated with greater disability. (Menendez et.al 2015, Pensak, M et al 2013). Splints generally have the potential to reinforce disability and secondary gain from this condition and maybe not useful and even harmful for certain patients.
Splint design in hand therapy practice for DeQuervains Tenosynovitis varies amongst practitioners and clinics. Factors to consider in splint design in this patient group are:
• Age
• Employment type
• Activity status
• BMI
• Irritability of condition
• Cost/affordability
Some splint design offerings include:
• Custom Made rigid Thermoplastic immobilising the wrist and thumb
• Semi-custom neoprene splint with mouldable thermoplastic insert ( radial gutter)
• Off the shelf semi-rigid splint. With plastic or metal inserts for reducing movement at the thumb and/or wrist
• Other
Splints are offered to patients to immobilise or significantly reduce the movement of the thumb and wrist in effort to “rest” the EPb/APL tendons and reduce pain and /or inflammation.
Many patients respond favourably to any of the above splints, however, some problems arise from the general design which immobilises the wrist and thumb in all rays of movement. These include :
• Wrist / thumb stiffness
• Aching
• Poor function and poor compliance
• Difficulty weaning from splint
• Dependence on splint
• Negative effects of immobilisation (especially associated with rigid splinting)
It is therefore desirable that the splint is for a short as period as possible to achieve symptom relief but also minimises the negative associations of disuse, poor function and maladaptive movement patterns.
A new splint design, first seen /published by Orfit, introduces the concept of controlled motion where the aggravating movement I.e wrist Radial deviation/ thumb extension for the EPb/APL is immobilised, but some wrist flexion and extension can occur with the splint on.
The proposed advantages of this splint could be:
• improved function of the immobilised limb due to less biomechanical limitations in the F/E plan of movement
• Reduced negative effects of immobilisation on thumb , wrist and upper limb generally due to some movement allowed at the wrist joint ( weakness, reduced muscle mass, joint stiffness, reduced tendon nutrition )
• Improved compliance due to less rigidity /impact on function
• Reduced dependence on splint and easier weaning off splint
This new splint design has been trialed on 3 patients with differing presentations:
- Acute presentation – < 2 weeks onset
- Chronic /recurrent presentation – 3 months since onset, 12 months from initial episode
- Subchronic – 8 weeks since onset
Acute presentation case study
- 2 weeks since onset
- No HCLA
- Ambulance officer
- Young 28-year-old active female
- Splinting- initial splint immobilising the wrist and thumb for 2 weeks then modified for controlled motion
- Rationale – the acute presentation with 8/10 pain and positive Finkelstein test with thumb opposition alone, painful wrist motion indicated that the tissues would benefit from a short period of immobilisation followed but controlled motion splint to allow return to normal function within the splint and without the biomechanical disadvantages of full immobilisation. Minimal time for disuse or neuroplastic changes.
Chronic/Recurrent presentation case study
- 48-year-old female
- Recurrent DeQuervains, 3 months duration, 12 months since previous episode
- Part-time Office worker
- Active mother of teenagers
- Rationale – at this stage, the condition will be of more degenerative nature, where traditional immobilisation and the negative effects of tendon weakness, poor nutrient exchange and joint stiffness, reduced forearm muscle mass and reduced strength will likely negatively effect tissues and outcome. The controlled motion splint combats these effects but still effectively rests the EPb/APL tendons. The improved movement in the splint means improved overall function and use of the arm, thereby limiting the “broken wing” fear-based behaviour pattern that can sometimes occur with recurrent symptoms and makes wearing from splinting difficult.
Subchronic – 8 weeks presentation case study
- 65 year old female
- Active retiree, gardening and house renovating
- Rationale – had attempted different versions of semi-rigid splinting without success and presented with hypersensitivity, poor behaviour patterns withholding movement at shoulder /elbow and wrist to minimise pain. Tissues in degenerative stage >> inflammatory therefore immobilisation likely to further deteriorate. An active lifestyle means controlled motion splint more likely to be tolerated but still limit aggravation of condition by preventing overuse of thumb/ wrist with activity.
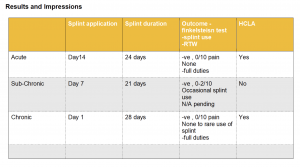
Results and Impressions
The CM splint was well tolerated by all patients, however the acute presentation needed pressure relief over radial styloid (theraputty and foam). All 3 presentations required splint modifications to reinforce the joins/hinges . The 2 patients that had experience with rigid splint 1st ( 7 days for subchronic, 14 days for acute) both preferred the CM splint. Clinically, the Finklestein’s test was negative on the 1st visit following introduction of the splint and remained that way until discharge. The inclusion of HCLA was beneficial in combination with splint for acute and chronic presentations. All patients received isometric wrist stability exercise concurrent with splint use and progressed to dynamic stability exercise ( disturbance based exercises) prior to discharge.
Clinical experience generally less time in a splint was needed to relieve symptoms than with usual splint designs.
Discussion
The CM splint has been a welcome addition in the armoury for treating this condition, however there are some things to consider regarding these results . The patients were carefully chosen for their open-minded attitudes and willingness to try something different which may have contributed to a positively skewed placebo effect. The inclusion of HCLA injection in 2/3 patients was also likely to have contributed to the success of the splint. The role of dynamic tape and use of exercise were not
independently compared for their value however all 3 patients received these as part of their treatment regime in addition to splinting.
It is proposed that because the splint design allows for some wrist motion in the flexion/extension plane it doesn’t restrict the patient functionally as much as a rigid splint. Neuroplastic changes that occur with immobilisation are minimised with this design and patients potentially are not as “disabled” by their splint and their behaviour was still essentially “normal”. Additionally, the deleterious effectors of immobilisation are minimised with this design but the essential aggravating movements are still minimised to allow symptom relief and in this case study, less overall time in the splint.
Fabricating the Controlled Motion Splint
The splint is a circumferential thumb spica splint that is halved and 3 hinges are attached to control the wrist motion.
Equipment
• thermoplastic
• Velcro -hook and loop
• Orficast strips x 3 or thermoplastic strips x 3 5-8 cm x 1cm
• Rivets – ( optional)
Instructions
1. Fabricate a forearm based circumferential thumb spica. **
2. Cut the handpiece from the forearm piece at the level of the radiocarpal joint
3. Roll edges of handpiece and forearm piece
– forearm piece can be positioned below the radial styloid or moulded over foam to minimise direct pressure over EPb/APL tendons at the retinaculum of the wrist
4. Attach Velcro strips to handpiece and forearm piece and place on patient.
5. Prepare Orficast strips
– need to be the length between the bottom of the handpiece and the top of the forearm piece, approximately 5-8cm
6. Using a pen, mark on the thermoplastic handpiece and forearm piece, the precise location for Orficast strips
– Volar Ulna border of handpiece attaches to Volar Ulna border of forearm piece
– Dorsal Ulna border of handpiece attaches to Dorsal Ulna border of forearm piece
– Radial border of handpiece. Attaches to radial border of forearm piece
7. Fit to patient as per usual
** A forearm based volar thumb spica can also be considered depending on therapist and patient preference and level of support needed.
Controlled Motion Splint – Allows wrist Extension and Flexion
Helpful hints
1. Pressure relief over radial styloid useful especially if v sensitive
2.Concurrent dynamic tape so thumb/wrist are supported and tactile feedback when not using splint
3. Instruct to use as needed only
4. It is better to make a circumferential splint in the 1st instance that can be easily cut down rather than trying to adapt a volar thumb spica if you think you might consider this design down the track from an initial appointment
References and recommended reading
Papa, J. A. (2012). Conservative management of De Quervain’s stenosing tenosynovitis: a case report. The Journal of the Canadian Chiropractic Association, 56(2), 112–120.
E Awan WA, Babur MN, Masood T. (2016)Effectiveness of therapeutic ultrasound with or without thumb spica splint in the management of De Quervain’s disease.J Back Musculoskelet Rehabil. 2016 Dec 23. doi: 10.3233/BMR-160591
Cavaleri R1, Schabrun SM1, Te M1, Chipchase LS2 (2016).Hand therapy versus corticosteroid injections in the treatment of de Quervain’s disease: A systematic review and meta-analysis. J Hand Ther. 2016 Jan-Mar;29(1):3-11. doi: 10.1016/j.jht.2015.10.004. Epub 2015 Nov 6.
Neiduski, R. (2016)Clinical Relevance Commentary on: Hand therapy versus corticosteroid injections in the treatment of de Quervain’s disease: A systematic review and meta-analysis.
J Hand Ther. 2016 Jan-Mar;29(1):12-3. doi: 10.1016/j.jht.2015.12.004. Epub 2015 Dec 1
Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B.(2009) Corticosteroid
Menendez, M.E., Thornton, E., Kent, S. et al. International Orthopaedics (SICOT) (2015) 39: 1563. https://doi-org.ipacez.nd.edu.au/10.1007/s00264-015-2 Prospective Randomised clinical trial of prescription of full time vs as desired for splint usage in DeQuervains tenosynovitis .
Duncan S, Flowers C. (2015). DeQuervains Tenosynovitis Chapter . Therapy of the Hand and Upper Extremity : Rehabilitation Protocols
Brandon E.EarpMDCarin H.HanBAW. EmersonFloydBATamara D.RozentalMDPhilip E.BlazarMD(2014)
de Quervain Tendinopathy: Survivorship and Prognostic Indicators of Recurrence Following A Single Corticosteroid Injection.The Journal of Hand Surgery. Volume 40, Issue 6
Mardani-Kivi, M, Mobarakeh, M, Bahrami, F, Hashemi-Motlagh,K, Saheb-Ekhtiari, K , Akhoondzadeh, N(2014)Corticosteroid Injection With or Without Thumb Spica Cast for de Quervain Tenosynovitis
The Journal of Hand Surgery, Volume 39, Issue 1, 2014, pp. 37-41
Illyas , A. MD(2009).Nonsurgical Treatment for de Quervain’s Tenosynovitis. The Journal of Hand.
Backstrom KM, Mobilization with movement as an adjunct intervention in a patient with complicated de Quervain’s tenosynovitis: a case report.(2002)J Orthop Sports Phys Ther. 2002 Mar;32(3):86-94; discussion 94-7.
Mehdinasab SA, Alemohammad SA. (2010)Methylprednisolone acetate injection plus casting versus casting alone for the treatment of de Quervain’s tenosynovitis.Arch Iran Med. 2010 Jul; 13(4):270-4.
Killian, M. L., Cavinatto, L., Galatz, L. M., & Thomopoulos, S. (2012). THE ROLE OF MECHANOBIOLOGY IN TENDON HEALING. Journal of Shoulder and Elbow Surgery, 21(2), 228–237. http://doi.org/10.1016/j.jse.2011.11.002
Pensak MJ1, Bayron J, Wolf JM. (2013) Current treatment of de Quervain tendinopathy.
J Hand Surg Am. 2013 Nov;38(11):2247-9